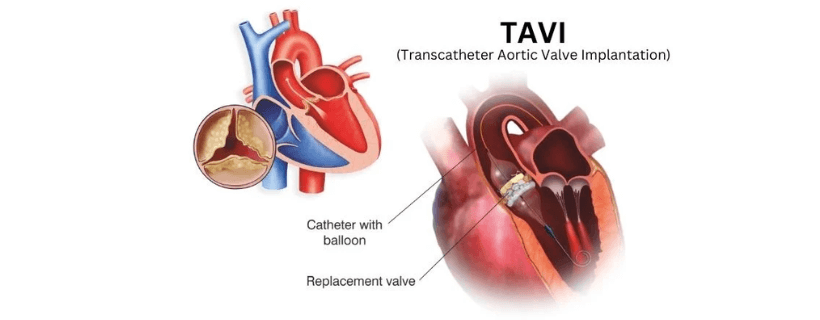
Transcatheter aortic valve implantation, often referred to as TAVI, is a minimally invasive technique that involves inserting a replacement valve into your heart. TAVI is also known as TAVR, which stands for transcatheter aortic valve replacement. TAVI procedures are currently a recognized and effective treatment for individuals with symptomatic severe aortic stenosis, and it is a viable alternative to surgery in some high-risk patients who cannot be operated on.
People with symptomatic aortic stenosis can benefit from TAVI as it can improve their quality of life and life expectancy while also lowering symptoms! The success rate for transcatheter aortic valve replacement is 90%, a significant rate! Early clinical research and trials indicated that among patients at higher risk for surgical problems, TAVI was more likely to be effective and less likely to result in death or serious complications.
What is Transcatheter Aortic Valve Implantation?
Transcatheter aortic valve implantationis an alternative to open heart surgery and is used as a medical technique that replaces the aortic valve in your heart. These days, the most popular method for replacing an aortic valve is this minimally invasive technique. The aortic valve is the last one of your heart’s four valves that regulate your blood flow to the entire body, and through that valve, your heart circulates blood to your aorta as well.
According to research, TAVI is often safer than surgical aortic valve replacement (SAVR) and produces results that are comparable to or superior to SAVR. If you have an increasing chance of heart failure because of aortic valve stenosis, you might need to have your aortic valve replaced through this procedure.
How is TAVI Performed?
The TAVI procedure for the heart is a complicated process that is handled very cautiously and delicately! You will be given either general anaesthesia (less common) or mild sedation (most frequent) before the start of the surgery, and even though both can prevent pain, mild sedation has a weaker impact.
A medical professional inserts a tube into your throat and attaches it to a breathing apparatus during general anaesthesia, and after the operation is complete, they remove the tube. What’s more, you will be given medication to avoid blood clots. TAVI is usually done inside the cath lab or hybrid OT with surgical backup.
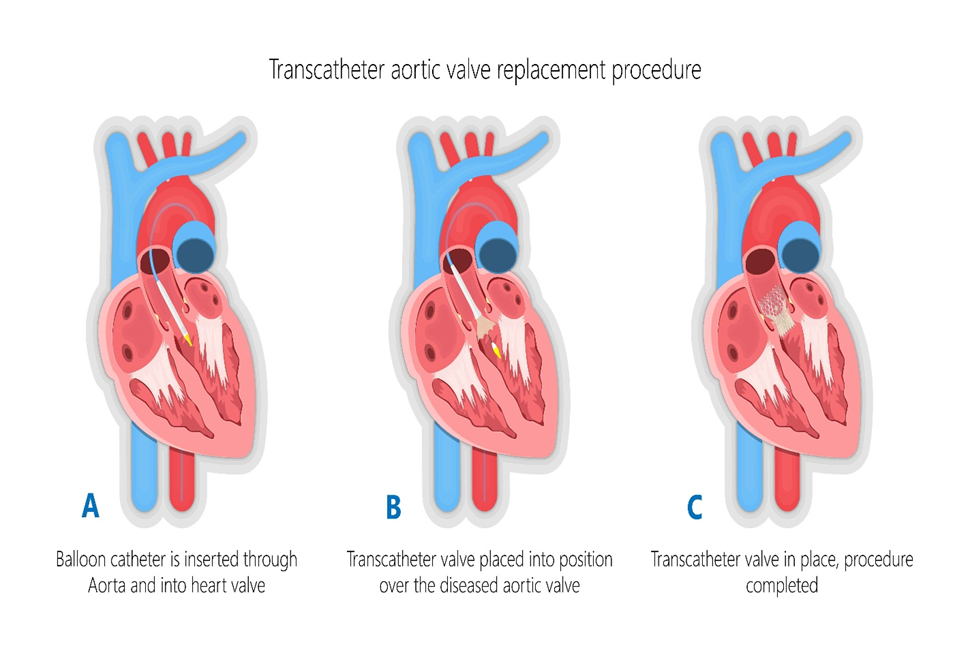
A cardiologist doing a transcatheter aortic valve implantation will use an antiseptic solution to clean the skin surrounding the surgery site. To access your aortic valve, the surgeon inserts a catheter into your leg artery and then takes it through your aorta to perform the procedure.
Throughout the surgery, your surgeon will insert more catheters into your heart to obtain measurements and X-ray images; in addition to that, the surgeon will guide either a balloon-expandable valve or a self-expanding valve through your old aortic valve and up the femoral artery catheter.
Your surgeon will then replace the old valve with the new one when it is positioned correctly. However, before removing the catheters, your doctor will take measurements and pictures to ensure your replacement valve functions as intended.
The function of the replacement valve is subsequently evaluated using transthoracic echocardiography. After completing the process, your physician will use a suture device that doesn’t require an incision to close your femoral artery.
What Happens After the TAVI Procedure?
To be closely monitored following your surgery, you can be admitted to the intensive care unit (ICU) of the hospital for the night, but remember, numerous factors determine how long you spend in the hospital for transcatheter aortic valve replacement recovery.
Some TAVI patients may return home the next day after the treatment!Fever, increasing discomfort and redness, swelling, and leaking or draining at the catheter site are all warning symptoms of infection. Following TAVI, several medications may be administered to patients.
- Anticoagulants – This medication aids in blood clot prevention, and your health status determines the length of time you may need to take this medication. Always remember to take medications exactly as prescribed.
- Antibiotics – These medications treat and prevent bacterial infections because artificial heart valves can become infected or adhere to germs. Most germs that cause heart valve infections originate in the mouth, but these infections can be avoided by taking appropriate care of your mouth and teeth!
Following TAVI, routine medical examinations and imaging tests are required to ensure the replacement valve is functioning as intended. Still, remember to inform your doctor of any new or worsening symptoms, such as:
- Light headedness
- Dizziness
- Swelling at the ankles
- Unexpected increase in weight
- Excessive fatigue
- Redness
- Swelling
Most importantly, you must seek immediate medical attention if you have chest tightness or pain, sudden shortness of breath, or if you faint.
The Health Risks of TAVI
Clinical studies have demonstrated the safety and efficacy of TAVI. However, there are some TAVI procedure risksassociated with the process, so let’s take a look.
| Valve leaks | This can happen when the replacement valve is too small, hasn’t expanded completely, or has calcium buildup interfering with it; however, more recent models being developed are more effective. |
| Kidney damage | Your kidneys may be harmed by the contrast dye used for imaging, although this is typically treatable. |
| Damage to your vessels | Putting catheters through your arteries may cause harm to them. |
| Pacemakers | Sometimes, valves that open during implantation might put pressure on the heart’s system, necessitating the use of a pacemaker because of the development of heart block. |
| Stroke | Some patients having TAVI have experienced a stroke, either during or shortly after the treatment. This is one of the seriouscomplications of the TAVI procedure, but the number of people who suffer from it is really small! |
Benefits of TAVI
Compared to surgery, a TAVI treatment offers several benefits, and for this reason, it is currently the most often used technique for aortic valve replacement.Among those benefits are:
- Less intrusive than open-heart surgery – Large incisions are made in your chest for the majority of cardiac procedures, and to do cardiac surgery, surgeons frequently need to elevate your rib cage or even break it apart. No internal organs or ribs need to be moved during TAVI; a tiny incision is made for this process.
- Recovery is easier – Your body will need less time to recover if the incisions are smaller, there will be less discomfort, and there will be a quicker recovery result.
- Shorter hospital stay -A hospital stay of several days is typically required following open heart surgery. However, your doctor could send you home the same day or the following day after transcatheter aortic valve implantation. The severity of your case, the time of your surgery, and your general health will all play a role in this.
Final Remarks
Transcatheter aortic valve implantation, or TAVI, is a minimally invasive surgery! This procedure has been performed on thousands of patients, and no matter your condition, it has significant advantages over open heart surgery, but if you are going for a TAVI surgery, selecting a practitioner who has extensive expertise doing this treatment will help increase the success rate.
If you are facing any heart-related conditions and need treatment for it, visit your nearest super-specialty hospital as soon as possible!
FAQs
1. What are the main benefits of TAVI/TAVR?
The procedure offers quicker recovery, reduced hospital stays, and fewer complications compared to open-heart surgery. It also significantly improves heart function and quality of life.
2. How long does the TAVI/TAVR procedure take?
The procedure typically takes 1-2 hours, depending on the complexity, and most patients are awake with light sedation during the process.
3. What is the recovery time after TAVI/TAVR?
Recovery is generally faster than open-heart surgery. Patients can often resume normal activities within a week, with full recovery in a few weeks.
4. Is TAVI/TAVR safe?
Yes, TAVI/TAVR is considered safe and is backed by extensive clinical studies. However, like any medical procedure, it carries risks, including bleeding, infection, or stroke.
5. Will I need blood thinners after TAVI/TAVR?
Most patients require blood-thinning medication temporarily to prevent clot formation. Your doctor will provide specific guidance based on your condition.