Laparoscopic surgery has revolutionized the treatment of gallbladder disease, offering a minimally invasive alternative to traditional open surgery. At GHC Superspeciality Hospital in Thane and Mumbra, we specialize in performing laparoscopic cholecystectomy to treat gallbladder conditions, such as gallstones and cholecystitis. This advanced technique not only improves patient outcomes but also enhances the overall patient experience by reducing recovery times, minimizing complications, and ensuring better post-surgery care.
In this blog, we’ll explore how laparoscopic surgery improves the treatment of gallbladder disease and why choosing GHC Superspeciality Hospital ensures the best possible results for patients in Thane and Mumbra.
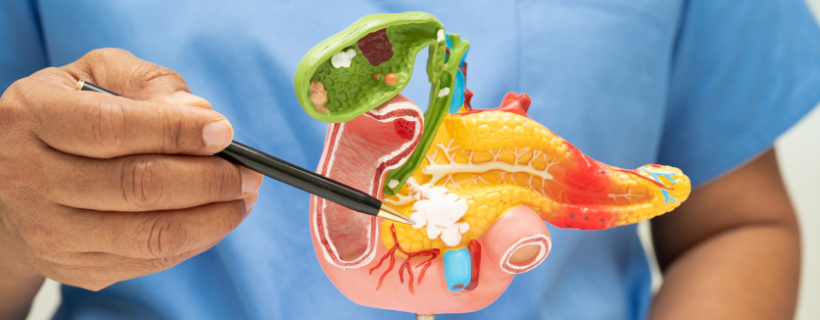
Understanding Gallbladder Disease
Gallbladder disease primarily refers to conditions that affect the gallbladder, an essential organ for bile storage and fat digestion. The most common gallbladder issues include gallstones (hardened deposits that form in the gallbladder) and cholecystitis (inflammation of the gallbladder).
Symptoms of gallbladder disease often include:
- Severe abdominal pain (especially after eating fatty meals)
- Nausea and vomiting
- Indigestion and bloating
If left untreated, gallbladder disease can lead to serious complications like gallbladder rupture or pancreatitis, requiring immediate medical intervention.
Traditional Treatment Options
Historically, gallbladder disease was treated through open surgery, which required large incisions and extended recovery periods. This method had a higher risk of infection and complications, especially for patients with pre-existing health conditions.
At GHC Superspeciality Hospital, we focus on the most modern techniques to provide the best patient outcomes, including laparoscopic surgery for gallbladder removal.
What is Laparoscopic Surgery?
A Minimally Invasive Approach
Laparoscopic surgery is a minimally invasive procedure that uses small incisions (typically 3-4) through which a camera and specialized instruments are inserted to perform the surgery. This approach allows surgeons to visualize the area with high precision, removing the gallbladder without making large cuts.
How Laparoscopic Surgery Differs from Traditional Surgery
Unlike open surgery, which requires a long incision across the abdomen, laparoscopic surgery uses tiny incisions. This not only reduces pain but also speeds up recovery. Laparoscopic surgery can be performed in a day-care surgery setting, meaning patients can return home the same day or the following day.
Benefits of Laparoscopic Surgery for Gallbladder Disease
- Faster Recovery Time
One of the main advantages of laparoscopic surgery is the reduced recovery time. Since the incisions are smaller and there is less trauma to the body, patients experience quicker healing. In most cases, patients can return to normal activities within 1-2 weeks as opposed to 6-8 weeks with traditional surgery.
- Reduced Risk of Infection
The small incisions used in laparoscopic surgery decrease the exposure of internal tissues to the external environment, leading to a significantly lower risk of infection compared to traditional open surgery.
- Less Pain and Scarring
Due to the minimally invasive nature of laparoscopic surgery, patients typically experience less post-operative pain. Additionally, the incisions are smaller, leading to minimal scarring and a more aesthetically pleasing result.
Improved Patient Outcomes at GHC Superspeciality Hospital
- Quicker Return to Daily Activities
At GHC Superspeciality Hospital in Thane and Mumbra, our laparoscopic gallbladder surgeries are designed to offer minimal disruption to your daily life. Patients can often resume work and normal activities much sooner than with traditional open surgery, which can be particularly beneficial for those with busy schedules or family obligations.
- Shorter Hospital Stays
Most patients undergoing laparoscopic gallbladder surgery are able to leave the hospital within 24-48 hours of the procedure. This not only saves time but also reduces the risk of hospital-acquired infections, providing a better overall recovery experience.
- Lower Risk of Complications
Laparoscopic surgery has a lower risk of complications like bleeding, infections, and bile leakage. At GHC Superspeciality Hospital, our highly skilled surgeons use advanced techniques to ensure the safest and most effective treatment for gallbladder disease.
Why Choose GHC Superspeciality Hospital for Laparoscopic Gallbladder Surgery?
- Expertise of Our Surgical Team
At GHC Superspeciality Hospital, we pride ourselves on having a team of highly experienced surgeons who specialize in laparoscopic surgeries. Our experts provide personalized care to ensure the best surgical outcomes for each patient. Our hospital is equipped with the latest state-of-the-art equipment, ensuring optimal results for gallbladder surgeries.
- Comprehensive Care and Support
From the initial consultation to post-surgery follow-up, we offer comprehensive care at every step of the treatment process. At GHC Superspeciality Hospital, patients receive continuous support and guidance to ensure smooth recovery.
The Laparoscopic Cholecystectomy Procedure
Laparoscopic cholecystectomy is the standard procedure for removing the gallbladder in patients suffering from gallbladder disease. The process typically involves the following steps:
- Anesthesia: The patient is given general anesthesia to ensure they are comfortable and pain-free throughout the procedure.
- Incision and Insertion of Laparoscope: A small incision is made near the belly button, and a laparoscope (a thin tube with a camera) is inserted to provide a clear view of the gallbladder.
- Insertion of Surgical Instruments: Additional small incisions are made to insert specialized surgical instruments. These instruments are used to carefully detach the gallbladder from its surrounding structures.
- Gallbladder Removal: The gallbladder is then removed through one of the small incisions.
- Closing the Incisions: Once the gallbladder is removed, the incisions are closed with sutures or staples.
Conclusion
Laparoscopic surgery for gallbladder disease has transformed the way patients receive treatment, offering significant advantages over traditional open surgery. At GHC Superspeciality Hospital in Thane and Mumbra, patients can access expert care from experienced surgeons who use the latest technology and techniques to ensure the best possible outcomes. With faster recovery times, minimal scarring, and lower risk of complications, laparoscopic surgery is an excellent choice for individuals suffering from gallbladder disease.
If you or a loved one is dealing with gallbladder disease and are seeking an effective, minimally invasive treatment option, consider consulting with the experts at GHC Superspeciality Hospital. Your path to recovery begins with the right care!